Neurosurgical Oncology Ward 3
Neurosurgical Oncology Ward 3
Neurosurgical Oncology Ward 3 (Middle-line skull base tumors and neuroendoscopy)
Specialized features
The Neurosurgical Oncology Ward 3 is characterized by the clinical application of neuroendoscopic technology. The annual number of neuroendoscopic surgeries exceeds 1200, and the quantity and quality of neuroendoscopic surgeries are leading domestically and internationally. Endoscopic neurosurgery is one of the critical technologies of minimally invasive Neurosurgery, which aims to give patients the best effect with minimal invasion. The operation method is to use special endoscopic instruments to complete high-quality surgical operations through the natural corridors or through small wounds. Under the leadership of academic leaders Professor Zhang Yazhuo and Director Gui Songbai, we are committed to the innovative development of neuroendoscopic technology and have formed a neuroendoscopic technology innovation team with independent technical characteristics. We have a group of young and middle-aged backbone experts, including Li Chuzhong, Geng Sumin, Zhao Peng, Bai Jiwei, Cao Lei, Liu Chunhui, Zhu Haibo, and Li Zhenye, etc. At the same time, the ward is also the unit where the Neuroendoscopic Training Base of the Chinese Medical Doctor Association is located, actively developing, training, and promoting clinical diagnosis and treatment techniques for middleline skull base tumors and neuroendoscopic techniques.
Treatment scope
I. Endoscopic skull base surgery
It is mainly used for the surgical treatment of lesions in the midline area of the skull base. The diseases primarily treated include pituitary tumor, chordoma, craniopharyngioma, meningioma in the midline area of the skull base, some lateral skull base lesions, cerebrospinal fluid leakage, and other skull base tumors with intracranial and extracranial communication. In addition, it has the following advantages:
1. Comprehensive surgical view, which can show blind areas and dead corners that the surgical microscope cannot reach
2. In deeper operative fields, neuro endoscopy can observe lesions at close range, providing better observation quality for deeper operative areas and better resolution clarity than microscopy.
3. Less surgical trauma
1. Pituitary tumors
Currently, endoscopic transnasal surgery is the preferred treatment for most pituitary tumors.
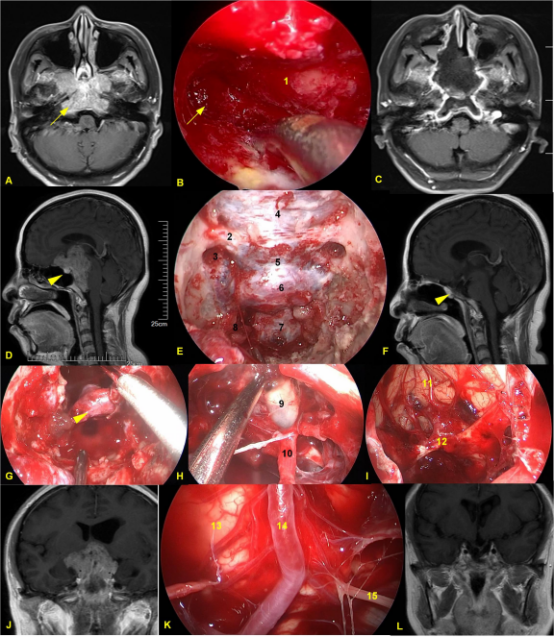
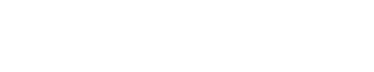
Figure 1. A-C,Pituitary adenoma with bone invasion. A. C preoperative and postoperative MRI. During the surgery, the bone of the jugular tubercle invaded by the tumor was removed. D-L Giant pituitary adenomas. D,F Pre-operation and 1 year post-operation MRI. E Intraoperative bone window exposure range. G.After tumor resection, the normal pituitary gland was preserved.H. After tumor resection, the third ventricle was opened. I The frontal lobe and Anterior communicating artery complex were exposed after tumor resection.K The brainstem and anterior pontine cistern were exposed. J,L. Pre-operation and 1 year post-operation MRI. 1 clivus; 2 Right optic canal; 3 optic canal-internal carotid artery recess; 4. The dura of the planum sphenoidale; 5 Dura of tuberculum sellae; 6. Dura m of sellar floor; 7. Clivus dura; 8. Para-clival internal carotid artery; 9 Third ventricle; 10 Pituitary stalk; 11 frontal gyrus; 12 Anterior communicating artery complex; 13 Brainstem; 14 Basilar artery; 15 Left abducens nerve. The yellow arrow shows the jugular tubercle invaded by the tumor; The untailed yellow arrow shows the normal pituitary gland.
2.Skull base Chordomas
Currently, endoscopic transnasal surgery is the treatment of choice for most chordomas.
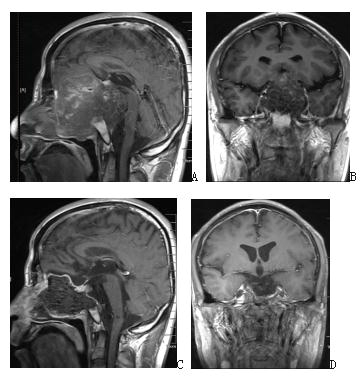
Figure 2. Enhanced MRI before surgery in A and B suggests recurrent giant full-slope chordoma; enhanced MRI after endoscopic transnasal surgery in C and D suggests complete tumor resection.
3. Craniopharyngioma
Transnasal endoscopic surgical resection is preferred for most craniopharyngiomas. It is minimally invasive, with a mild reaction, slight damage to vision and endocrine, and rapid patient recovery.
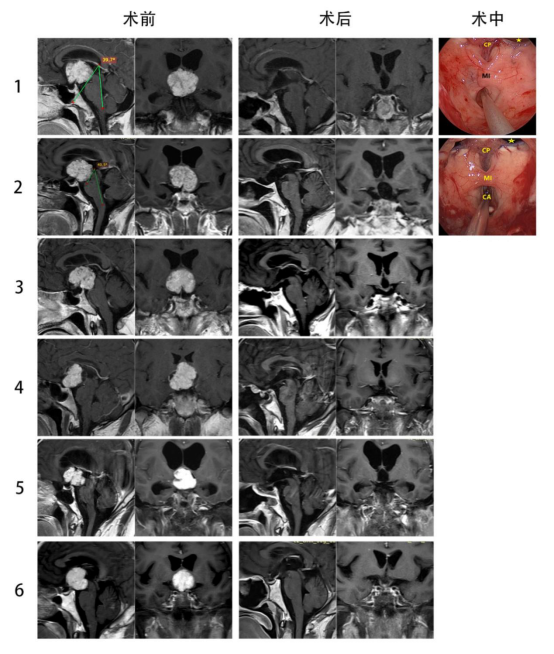
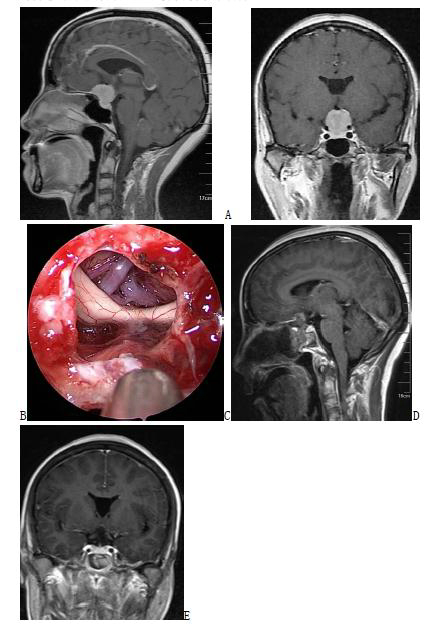
Figure 3. A and B Enhanced MRI before surgery suggest suprasellar craniopharyngioma; C Intraoperative screenshot suggests complete resection of the tumor, which can be seen in the three ventricles and the superior port of the midbrain aqueduct; D and E Enhanced MRI after endoscopic transnasal surgery, suggesting complete resection of the tumor.
4. Saddle-nodal meningioma
Some saddle-nodal meningiomas are suitable for transnasal endoscopic surgical resection.
Figure 4. A and B preoperative enhanced MRI; C intraoperative screenshot suggest complete tumor resection and visualization of the pituitary stalk, optic cross, and anterior cerebral artery; D and E post endoscopic transnasal surgical MRI suggest complete tumor resection.
II. Endoscopic Ventricular Brain Pool Surgery
At present, endoscopic ventricular brain pool surgery is mainly used for the surgical treatment of hydrocephalus, intracranial cysts, intracerebroventricular tumors, and tumors in the pineal region. It has the following advantages: (1) treatment of ventricular and brain pool diseases in the central part of the brain with tiny incisions and skull drilling, which is far less traumatic than traditional craniotomy; (2) deep in the brain, relying on the high resolution of the endoscope, a clear and magnified surgical field can be obtained, making the surgery more delicate; (3) safe and reliable, and the patient recovers quickly. (4) It avoids many complications of shunt surgery.
1. hydrocephalus (preferred neuro-endoscopic surgical treatment)
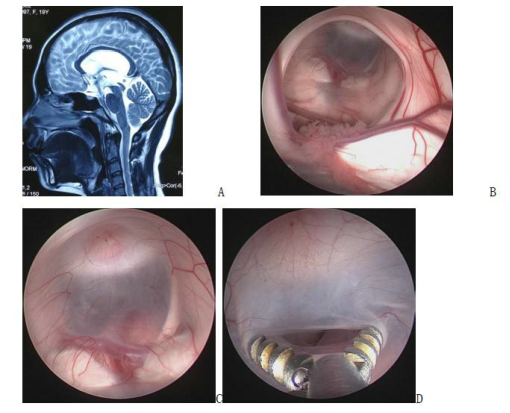
Figure 5. A preoperative magnetic resonance image; B intraoperative screenshot, endoscopically visible periventricular foramen structures; C, D base of the three ventricles and fistula (basilar artery visible below the fistula)
2. lateral fissure cyst (preferred neuro-endoscopic surgical treatment)
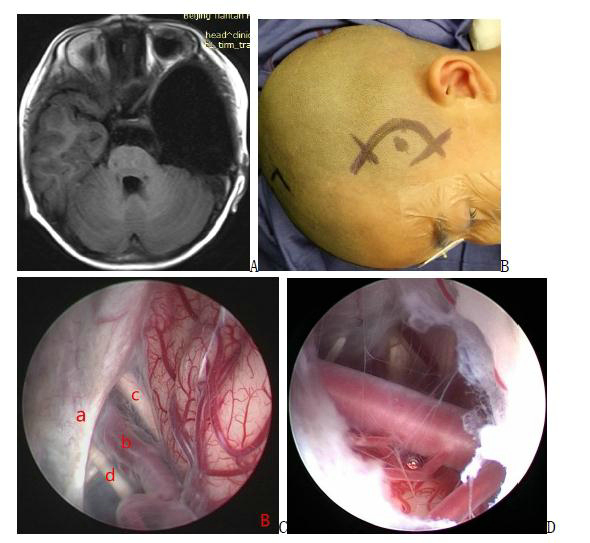
Figure 6. a pre-surgical MRI image; b illustration of scalp incision; c intraoperative screenshot, endoscopic view of 3 alternative fistula sites between the cyst and the basal pool: between the moto neurotic nerve and the cerebellar curtain margin; between the moto neurotic nerve and the internal carotid artery; and between the internal carotid artery and the optic nerve; d the basilar artery is visible below after fistula. a: cerebellar curtain b: internal carotid artery c: optic nerve d: moto neurotic nerve
3. tetraploid pool cyst (preferred neuro-endoscopic surgical treatment)
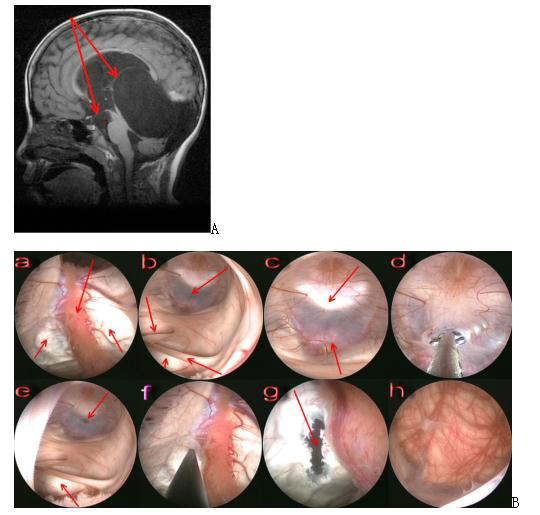
Figure 7. A Preoperative magnetic resonance image shows the arachnoid cyst of the tegmental pool protruding upward into the lateral ventricle, with arrows indicating the direction of the fistula at the base of the third ventricle as well as the cyst-lateral ventricle fistula; B Intraoperative screenshot, endoscopic view of the surgical steps for the arachnoid cyst of the tegmental pool. a: endoscopic entry into the lateral ventricle, with bilateral arrows below indicating the top of the cyst protruding into the lateral ventricle and arrows above indicating the choroid plexus; b: endoscopic entry into the third ventricle, with the upper right arrow indicating the floor of the third ventricle, the lower right arrow indicating the middle mass being stretched and elongated, the upper left arrow indicating the superior port of the catheter being squeezed closed, and the lower left arrow indicating the wall of the cyst protruding into the third ventricle; c: floor of the third ventricle, with the upper arrow indicating the dorsal saddle and the lower arrow indicating the basilar artery; d: fistula of the floor of the third ventricle; e: after fistula of the floor of the third ventricle, with the upper arrow indicating the fistula f: fistula at the top of the cyst protruding into the lateral ventricle; g: arrow indicating the site of the fistula; h: endoscope entering the cyst through the fistula and the superior surface of the cerebellum below is visible.
4. suprasellar pool cyst (preferred neuro-endoscopic surgical treatment)
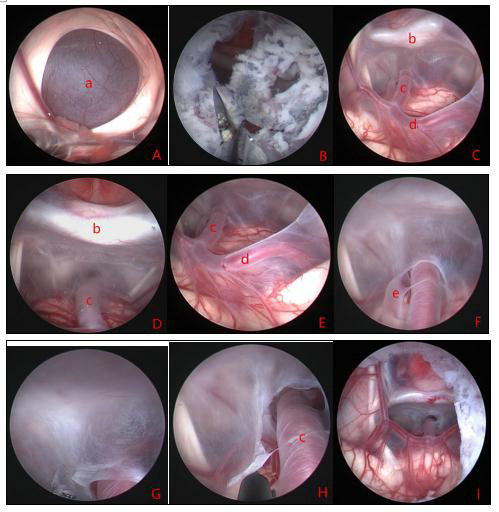
Figure 8. shows the intraoperative view of a suprasellar cyst with hydrocephalus. a: top of the suprasellar cyst; b: top fistula of the cyst; c, d, e: entry into the cyst through the top fistula, with the anatomy of the cyst's interior visible; f: fissure flap next to the basilar artery at the base of the cyst; g, h: fistula of the bottom wall of the cyst; i: bottom fistula completed, with the fistula above and below viewed from the lateral ventricle. a: cyst wall b: dorsal saddle c: basilar artery d: posterior cerebral artery e: fissure flap
5. lateral ventricular tumor
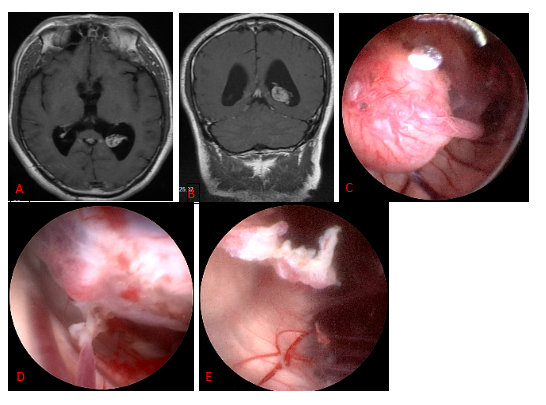
Figure 9. a, b: preoperative image of choroid plexus papilloma in the triangular region; c: intraoperative view of the tumor and the blood supply artery; d: electrocoagulation of the blood supply artery; e: after complete total resection of the tumor.
6. interventricular foramen area tumor
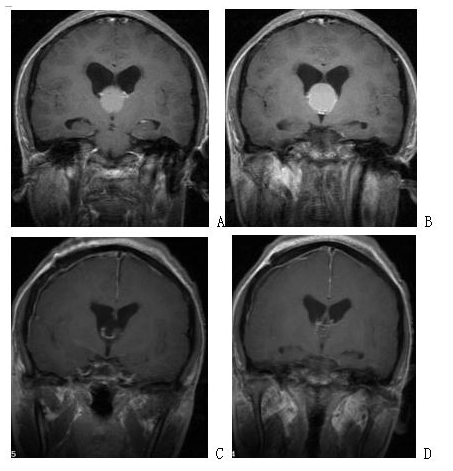
Figure 10. preoperative and postoperative imaging of endoscopic resection of interventricular foramen gumbo cyst via lateral ventricular frontal horn-interventricular foramen approach. A and B: preoperative images; c and d: postoperative images showing complete tumor resection.
7. posterior tumor of the three ventricles
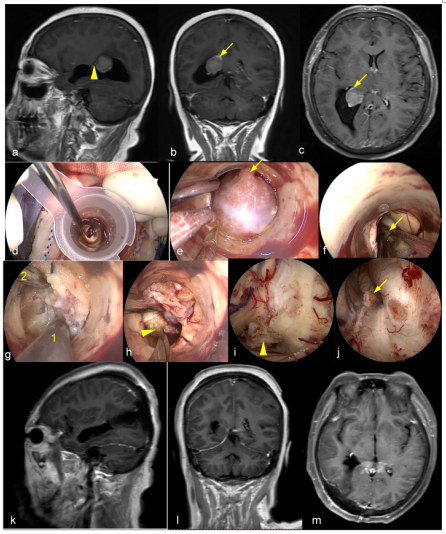
Figure 11. Endoscopic trans-endoport resection of trigone meningioma. a-c,Pre operative MRI showed meningioma in the left ventricular trigone area. d, Endoport Implantation; e,Confirm the origin of the tumor from the choroid plexus; f,Electrocautery of the choroid plexus of tumor origin; g,Resection of tumor by super absorption; h,After tumor volume reduction, electrocautize and cut off the adhesion with the choroid plexus; i,The choroid plexus extending towards the temporal angle of the lateral ventricle can be observed under water environment; h,The choroid plexus extending towards the atrium of the lateral ventricle. k-m,Postoperative MRI showed complete tumor resection. The arrow shows the choroidal plexus extending to the atrium of the lateral ventricle; The tailless arrow shows the choroidal plexus extending from the temporal angle of the lateral ventricle; 1 suction tube; 2 super absorption.
8. Endoscopic extra-operative technique for resection of lateral ventricular central astrocytoma
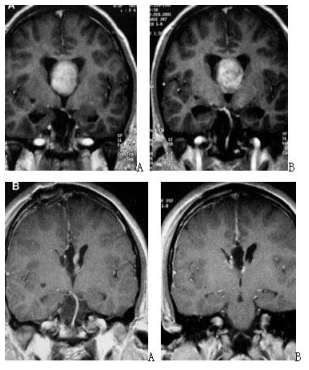
Figure 12. A and B preoperative images; C and D postoperative images.
III. Endoscopic transcranial surgery
The diseases such as brain parenchymal tumors, parafascicular meningioma, and epidermoid cysts are resected using micro-invasive, extra comic surgical, and epi-optic techniques. It has the advantages of minimal surgical trauma and quick recovery.
Scientific Research Technology
Since its establishment, the team has focused on the following four key directions: 1) primary and clinical research on the occurrence and development mechanism of pituitary tumors and modern treatment methods; 2) primary and clinical research on the occurrence and development mechanism of chordoma and modern treatment methods; 3) research on the fine localization of key functions of the human brain and multimodal imaging, and has applied for and undertaken national key special projects, special projects of the National Health Planning Commission, key research projects, the National Natural Science Foundation of China, and major research projects in Beijing, We have applied for and undertaken 53 national key projects, National Natural Science Foundation of China, major research projects in Beijing, and various provincial and ministerial level research projects. As a result, we have the largest specimen bank of pituitary tumors and chordomas in China and a comprehensive and systematic system of longitudinal research on pituitary tumors and chordomas. 4) Endoscopic transnasal surgery for craniopharyngioma and basic and clinical research on craniopharyngioma.
Honors received
2012, Beijing Science and Technology Award, Second Prize
2003, Beijing Science and Technology Award, Third Prize
Beijing Science and Technology Progress Award, Third Prize, 2002
Beijing Science and Technology Progress Award, Second Prize, 2000
2004, China Medical Award, Third Prize
Neurosurgical Oncology Ward 3Neurosurgical Oncology Ward 3 (Middle-line skull base tumors and neuroendoscopy) Specialized features The Neurosurgical Oncology Ward 3 is characterized by the clinical application of neuroendoscopic technology. The annual number of neuroendoscopic surgeries exceeds 1200, and the quantity and quality of neuroendoscopic surgeries are leading domestically and internatio…